Introduction - Glofitamab is a CD20-directed CD3 T-cell engager that has recently been approved by the FDA for relapsed and refractory diffuse large B cell lymphoma (R/R DLBCL). The approval was based on a pivotal phase II study including 154 patients with a median of 3 lines of treatment (a third post chimeric antigen receptor T (CAR-T) cell therapy) demonstrating an overall response rate (ORR) and complete response (CR) rate of 52% and 39%, respectively 1. However real-life data is still lacking. The present study was aimed to determine the efficacy and safety of glofitamab in real-life settings.
Methods -A retrospective multicenter study including consecutive patients aged 18 years and older with R/R DLBCL, treated through a national compassionate program with at least 1 dose of glofitamab, after failing at least three lines of therapy. The first patient was recruited in September 2020 till January 2023. Outcomes included ORR and CR, defined by the Lugano criteria; progression free survival (PFS) and overall survival (OS), defined from the day of obinutuzimab infusion until event; cytokine release syndrome (CRS) and immune effector cells-associated neurotoxicity syndrome (ICANS) were defined by the ASTCT consensus 2019. Risk factors for PFS and OS were identified by univariate and multivariate analyses, using logistic regression.
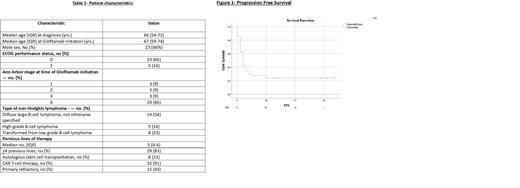
Results - A total of 35 patients treated in 6 Israeli centers, were included. Median age at the time of initiation of glofitamab was 67 years (59-74) and 66% of the patients were males. The median number of previous therapies was 5 (IQR, 4-6) and 83% received more than 3 previous lines of therapy. 43% were primary refractory, all but 3 received CAR-T cell therapy (91%) and 23% underwent autologous stem cell transplantation (Table 1). Median follow up was 34 months (IQR, 18-57). Outcomes: 34% achieved ORR with 14% achieving CR. Median PFS and OS was 2 (IQR, 1-6) and 4 months (IQR, 2-10), respectively (Figure 1). At the end of follow up - 12 (34%) patients survived, 21 died and 2 patients were lost to follow- up. Causes of death included disease progression in 15 patients and infections in 6. Treatment was discontinued earlier than 12 cycles in 86%, mostly due to progressive disease (76%), and 24% due to infections (3 - COVID-19; 3- bacterial). Adverse events included CRS in 37% - all grade 1-2. 2 patients developed grade 1 ICANS. In a multivariate analysis including age, male, bulky disease, elevated LDH and CRS, only male sex was found to be significant risk factor for PFS and OS (p=0.02, p=0.04 respectively).
Conclusions - In this real-life cohort of R/R DLBCL, glofitamab showed less efficacy than in the pivotal study. This might be due to the more heavily pretreated patients in our series with nearly all patients post CAR-T. Nevertheless, toxicity in our real-life analysis was better than reported in the pivotal study, supporting the role of glofitamab in R/R DLBCL patients.
References-
1. Dickinson et al. Glofitamab for Relapsed or Refractory Diffuse Large B-Cell Lymphoma. NEJM 2022;387:2220-31
Disclosures
Gurion:ABBVIE: Honoraria; TAKEDA: Honoraria; MEDISON: Honoraria; GILHEAD: Honoraria; NOVARTIS: Honoraria; ROCHE: Honoraria. Avivi Mazza:AbbVie: Honoraria. Horowitz:F. Hoffmann-La Roche Ltd: Research Funding; F. Hoffmann-La Roche Ltd: Honoraria. Raanani:Janssen: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Novartis: Consultancy, Research Funding. Nachmias:AbbVie, Medison, Astellas: Consultancy, Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal